When 65-year-old retired Ramesh first came to the hospital could barely hobble to the gate of his house without stabbing pain in his calves. His toes had developed dark patches that refused to heal. “The doctors said if things didn’t improve, I might even lose my foot or leg,” he recalls. He had a long block in his thigh artery.
Instead of preparing him for a stent or bypass surgery, the interventional radiology team offered something new: an angioplasty that clears the artery but leaves no permanent implant inside. A tiny device shaved away the hardened plaque choking his artery, and then a special drug-coated balloon was inflated for a minute. Blood flow returned, his pain eased, and weeks later, his wound began to heal.
“I’m walking to the market again,” he says with a smile. “And the best part—no metal stuck inside my leg.”
Why legs lose their lifeline
Blocked arteries in the legs—what doctors call peripheral artery disease (PAD)—are more common than most people realise. It is the same process as heart blockages, but here it strikes the arteries of the thighs, knees, and calves.
Cholesterol and calcium build up like lime scale in an old water pipe. At first, you may feel cramps in your calves when you walk. Later, pain creeps in even at night. In the worst cases, small cuts on the foot do not heal, turning into ulcers or even gangrene.
In India, with diabetes spreading fast, doctors are seeing more and more patients like Ramesh. One in five diabetics may already have narrowed arteries in their legs—even if they do not know it.
The old fix: Stents
For years, the standard answer was stents—tiny wire tubes that hold the artery open. Stents save lives and remain vital in many situations. However, in the legs, they have their quirks.
Leg arteries bend every time you sit, walk, or squat. Stents are made of metal; they do not always like bending. Over time, they can kink, fracture, or cause scar tissue to grow inside them again. In addition, if a future surgery is needed, having a long piece of metal in the artery can complicate things.
The new idea: “Leave nothing behind”
Enter the stent-free strategy. The idea is simple: fix the blockage, deliver medicine to keep it open, but do not leave a permanent implant inside.
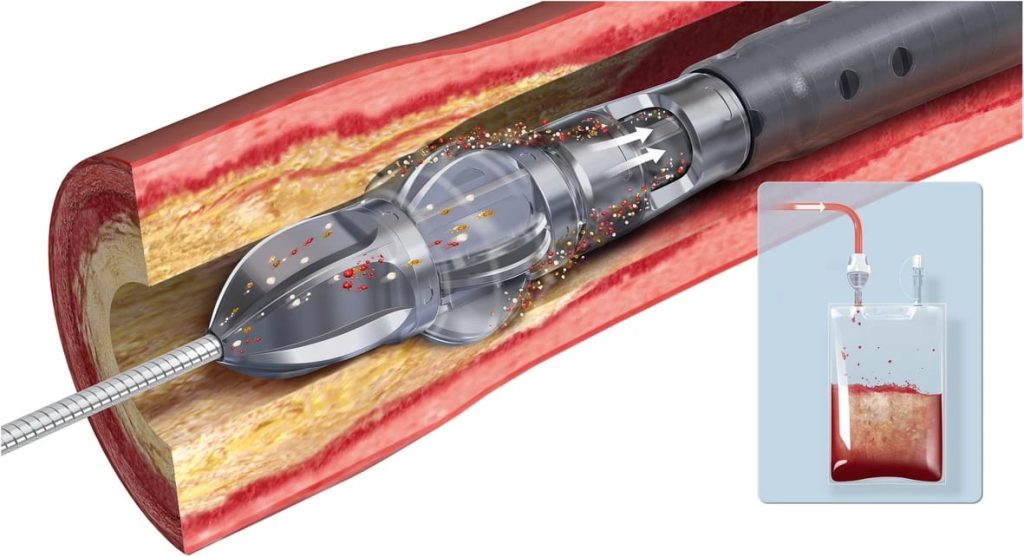
Doctors now have tools called atherectomy devices—think of them as gentle “drills” or “shavers”—that can carefully remove the crusty deposits clogging the vessel. Once the artery is cleaned out, a drug-coated balloon is inflated. Instead of simply stretching the artery, this balloon delivers medicine directly into the vessel wall, discouraging scar tissue from growing back.
The balloon is then removed, leaving behind nothing but a freer-flowing artery.
Why patients like it
- No permanent implant: Nothing left behind to fracture, shift, or complicate future surgery.
- More natural movement: The artery can bend and flex as it always has.
- Lower repeat procedures: Because the drug reduces re-narrowing, patients often get longer relief.
- Peace of mind: For many, it feels less invasive and “lighter” than living with a stent.
Dr. Charudutt Sambhaji, Vascular & Interventional Radiologist at Manipal Hospital Goa, explains: “We are not anti-stent. Stents save lives. However, where we can, we prefer to restore flow without leaving anything behind. It gives patients freedom and preserves options for the future.”
However, it is not a magic wand
Every treatment has another side. Sometimes the artery tears after ballooning, and a stent is still needed as a “rescue.” Sometimes plaque debris breaks off, so doctors use filters to catch it. Not every blockage can be handled this way—very long or complex ones may still need a stent or bypass.
In addition, the patient’s own choices matter hugely. If smoking continues or diabetes remains uncontrolled, even the best procedure can fail.
What patients can expect
Before: Simple tests like a Doppler scan or CT angiogram map the blockages. Medicines for blood pressure, sugar, and cholesterol are optimised.
The procedure is performed under local anaesthesia; a tiny puncture in the groin allows the doctor to pass wires and devices. Atherectomy removes plaque, and then the drug-coated balloon is inflated for about a minute. Most patients do not feel pain beyond mild pressure.
Often, you are walking the same day. You go home in one or two days. Medicines continue, and lifestyle changes begin. Follow-up scans at a few months check that the artery is still open.
A global debate and reassurance
A few years ago, headlines raised fears that the drug (paclitaxel) used on these balloons might increase long-term risk of death. Patients were understandably worried. However, after reviewing mountains of new data, the U.S. FDA and other global bodies concluded the treatment is safe when used properly.
Meanwhile, a new generation of balloons coated with sirolimus—another drug used safely in heart stents—has arrived, giving doctors and patients more options.
A matter of teamwork
The stent less approach is just one piece of the puzzle. Success also depends on:
- Kicking the habit: Smoking is PAD’s biggest enemy.
- Exercise: Walking itself improves blood flow by building tiny bypass vessels in the legs.
- Foot care: Especially for diabetics, daily inspection prevents small wounds from turning deadly.
- Medications: Blood thinners, statins, and sugar control remain the unsung heroes.
Dr. Charudutt Sambhaji adds: “The best device in the world can’t undo the harm of cigarettes or uncontrolled diabetes. We need patients to partner with us.”
The road ahead
Researchers are working on smarter balloons that release medicine more precisely, safer atherectomy tools that generate less debris, and even “bioabsorbable” scaffolds that vanish after doing their job.
Hospitals in India’s metros and large towns are increasingly offering this treatment. Awareness among patients, though, lags behind. Many only arrive when the disease is advanced.
How to know if you should ask about it
Pain in your calves or thighs when you walk, that eases with rest?
Wounds on your feet that do not heal?
Cold or discoloured toes?
These are red flags. See a specialist—an interventional radiologist, who precisely diagnoses and treats PAD. Ask if your artery anatomy makes you a candidate for drug-coated balloon angioplasty with or without atherectomy.
A second chance at steps
For Ramesh, the procedure was not just about saving his leg. It was about regaining his independence.
“Before, I felt like a burden. My family had to fetch everything for me,” he says. “Now, I take my grandson to the park. I walk beside him. That’s freedom.”
Moreover, that, ultimately, is what this stent-free revolution in angioplasty is about—not just technology, but giving people back their steps, their dignity, and their lives.

